
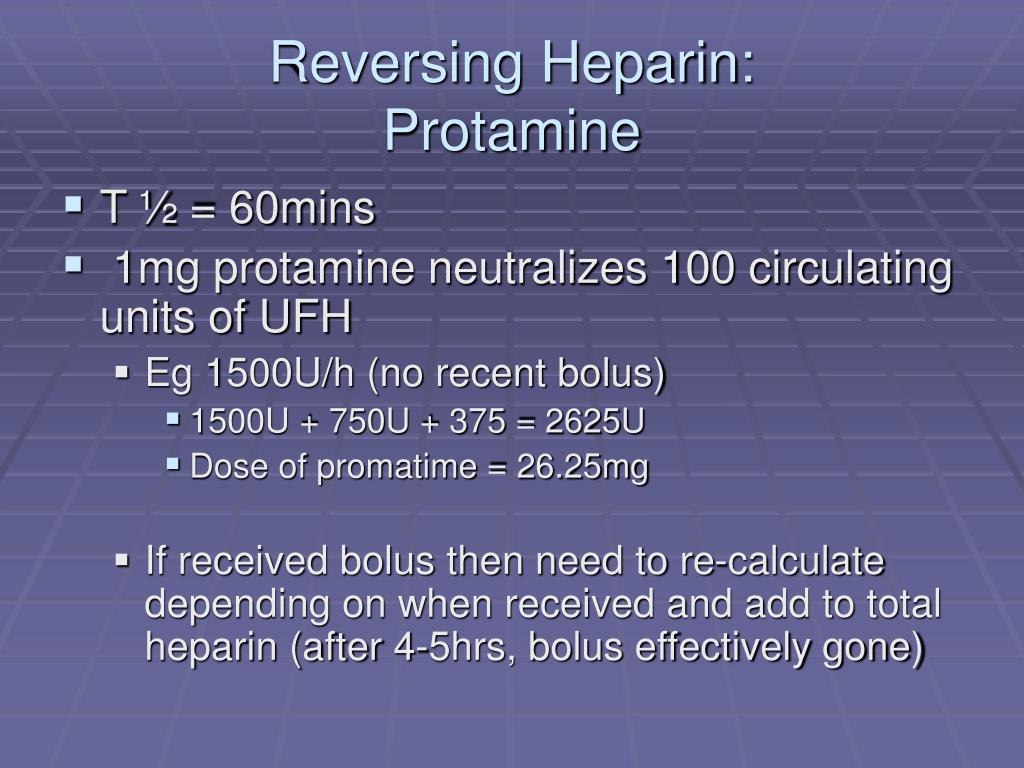
American College of Chest Physicians guidelines suggest using protamine sulfate to neutralize LMWH when necessary, although they give no specific recommendations on managing LMWH overdose. Protamine sulfate forms a stable complex with heparin, neutralizing its anticoagulant effect. He underwent an uncomplicated wound closure 15 days later. Two days after fasciotomy, we started the patient on VTE prophylaxis with dalteparin 5000 units subcutaneous daily, given his high thrombotic risk. During the period before and after the fasciotomy, the patient received three 50 mg doses of protamine sulfate, with the third dose in response to bleeding from the surgical site, after which hemostasis occurred. The plastic surgery service measured the pressure in his left anterior arm compartment, finding it to be elevated at 30 (normal 0–8) mm Hg, confirming a diagnosis of anterior compartment syndrome, which we attributed to a hematoma after veni-puncture, and subsequently performed an urgent bedside fasciotomy.įigure 1 shows a timeline of clinical events, coagulation blood tests and treatment. Examination showed arm edema, antecubital fossa ecchymosis surrounding a venipuncture site and a weak radial pulse. The internal medicine service admitted the patient, with support from the hematology and thrombosis service, and treated him with prophylactic intravenous protamine sulfate 50 mg every 6 hours and oral tranexamic acid 500 mg every 8 hours.Įighteen hours after his overdose, the patient developed progressive left arm pain.
The patient’s rivaroxaban level, measured by a drug-specific anti-Xa assay (Diagnostica Stago, Asnières sur Seine, France), was 351 (expected therapeutic range 182–408) ng/mL. Initial blood work results showed hemoglobin of 121 (normal 130–180) g/L, creatinine of 99 (normal 60–110) μmol/L, estimated glomerular filtration rate (GFR) of 81 (normal > 60) mL/min, international normalized ratio of 1.6 (normal 0.8–1.2), activated partial thromboplastin time (aPTT) of > 150 (normal 22–35) seconds, and LMWH anti-Xa level of 8.94 (therapeutic range 0.5–1.0) U/mL.
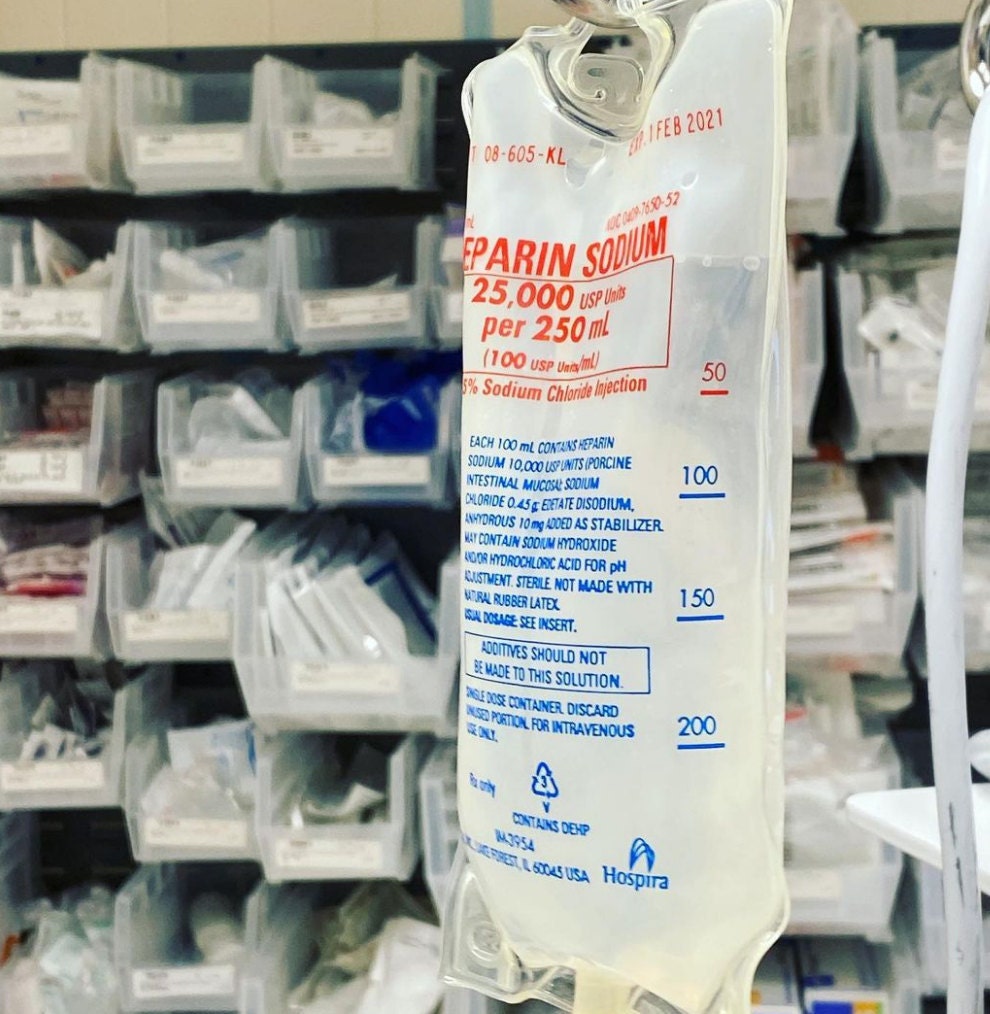
The patient’s vital signs were stable, and we observed no evidence of bleeding other than bruising around multiple abdominal injection sites. He had taken his last dose of rivaroxaban 3 days before the current presentation. The injected dalteparin was left over from a previous prescription for 15 000 units daily. Previously, he had switched among several anti-coagulants owing to intolerance or breakthrough thrombosis, including warfarin, various preparations of low-molecular-weight heparin (LMWH) and, most recently, rivaroxaban.
The patient’s medical history included depression, heterozygous factor V Leiden mutation and recurrent venous thromboembolism (VTE).
PROTAMINE ANTIDOTE FOR HEPARIN SERIAL
Serial monitoring of LMWH anti-Xa levels or activated partial thromboplastin time or both may help to guide therapy.Ī 42-year-old man presented to the emergency department 2 hours after self-injecting 225 000 units of dalteparin (15 prefilled 15 000-unit vials) with intent to self-harm.


 0 kommentar(er)
0 kommentar(er)
